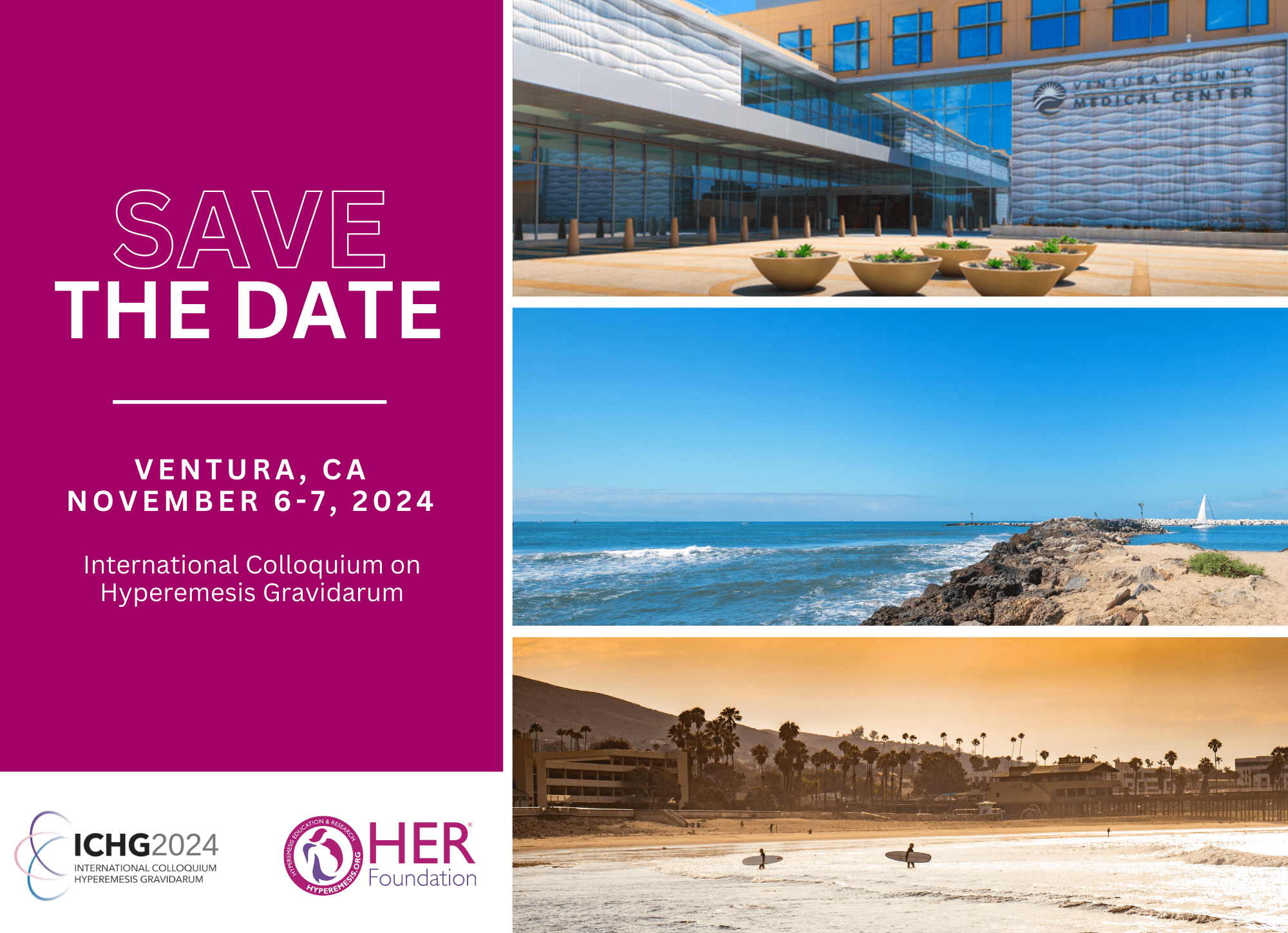
Join us November 6-7, 2024, in Ventura, California (near Los Angeles), for ICHG 2024, two days of engaging with top scientists and clinicians specializing in HG management.
Bringing together the world’s leading researchers in hyperemesis gravidarum, this two-day event in the heart of the Golden State will be an excellent opportunity for delegates to hear about the latest research developments and innovative treatments for this complex condition. Charities and patients will have opportunities to engage as well.
We will be accepting submissions for a limited number of late-breaking abstract presentations with a deadline of September 15th. A late-breaking abstract is an abstract that contains new information that was not yet known or fully available by the original annual abstract submission deadline of April 1st. Application coming soon.
If you have any queries about the ICHG 2024 conference, please contact Aimee Brecht-Doscher.
Featured Speakers
- Professor Stephen O’Rahilly
- Dr Marlena Fejzo
- Dr Marc Vaudel
- Dr Fanos Yeshanew Ayele
- Dr Rachel Carmen Caesar
- Dr Anne Ostenfeld
- Dr Eileen O’Brien
- Dr Aimee Brecht-Doscher
Scholarships
Attendees from low-middle income countries can apply to have most expenses covered. Those from other countries may apply for travel costs only. Deadline: June 15th, 2024
Share the Facts About HG
- HG, hyperemesis gravidarum, is a pregnancy disease marked by weight loss, malnutrition, and dehydration due to severe nausea and/or vomiting.
- HG is not the “morning sickness” of healthy, normal pregnancies. It is a distinct diagnosis marked by severe and relentless symptoms that pose significant risks to the health of both mom and baby. Over 1/3rd of HG babies do not make it to term.
- HG babies are at increased risk for low birth weight, small size for gestational age, and preterm birth. In utero exposure to HG is linked to a 3.6-fold increased risk of emotional/behavioral & developmental disorders, and autism. Up to 15% of HG pregnancies end due to therapeutic terminations, citing “no hope for relief.” Current treatments are not always adequate to prevent termination of these wanted pregnancies.
- Mothers with more severe HG can experience pneumothorax, organ rupture, retinal detachment and blindness, eardrum and jaw damage, rib fractures, esophageal tears, the neurological syndrome Wernicke’s encephalopathy, or even death.
- 18% of women report full criteria of post-traumatic stress syndrome (PTSS) following an HG pregnancy. More than half of mothers have post-traumatic stress symptoms.
- In 2016, the nearly 400,000 emergency and inpatient visits for HG in the U.S. cost more than $3,000,000,000. Outpatient treatment, medications, and nutritional therapy were additional.
- HG is the leading cause of hospitalization in early pregnancy, and is second only to preterm labor as the most common overall cause of hospitalization during pregnancy.
©2023 HER Foundation. All rights reserved.