About HG for Healthcare Providers is to provide you with information about HG, so you can better understand and support your patient. You can scroll down or click on the links:
Overview of HG
Hyperemesis gravidarum (HG) is a severe form of nausea and vomiting in pregnancy. It is generally described as unrelenting, excessive pregnancy-related nausea and/or vomiting that prevents adequate intake of food and fluids. HG is the leading cause of hospitalization during early pregnancy, and second to premature labor as the leading cause overall during pregnancy.
Severe and/or inadequately treated vomiting in pregnancy
If severe and/or inadequately treated, it is often associated with:
- loss of greater than 5% of pre-pregnancy body weight (usually over 10%)
- dehydration and production of ketones*
- nutritional deficiencies
- metabolic imbalances
- severe fatigue and debility
- depression/anxiety and trauma
- premature labor/delivery
- adverse fetal complications
(*Ketones are NOT always produced during HG thus ketones are not a required criteria for a diagnosis of HG.)
Occurrence
HG is the leading cause of hospitalization in early pregnancy and second overall next to premature labor/delivery. Incidence in the United States is poorly tracked and thus unknown, but often quoted from 0.5-2% though these use different criteria for diagnosis. Nearly 400,000 inpatient and emergency visits for HG occur annually in the USA alone, and the number is rising as inpatient visits decline with the focus on cost reduction in health care. With the majority of women no longer admitted to the hospital, the true incidence of HG is unknown and likely several times greater than estimated. It is not actually a rare disorder.
If adequate and compassionate treatment are not offered, a mother can suffer greatly and may even have acute or chronic anxiety and/or depression from the trauma of incessant nausea and vomiting, along with fears of death or loss of her child.
Duration
HG usually extends beyond the first trimester and may resolve by 21 weeks; however, it can last the entire pregnancy in less than half of women. Complications of vomiting (e.g. gastric ulcers, esophageal tears and bleeding, malnutrition, etc.) may also contribute to and worsen ongoing nausea.
Severity
Distinct from the mild and short-lived “morning sickness” common to most healthy pregnancies, HG does not look the same for every woman. There is a range of different experiences, from mild to moderate to severe. HG is the leading cause of hospitalization during early pregnancy, and second to premature labor as the leading cause overall during pregnancy.
What is Hyperemesis Gravidarum (HG)?
HG is hyperemesis gravidarum: a potentially life-threatening pregnancy disease that may cause weight loss, malnutrition, dehydration, and debility due to severe nausea and vomiting, and may cause long-term health issues for mom and baby.
Comparison of Morning Sickness and HG
| Area Impacted: | Hyperemesis Gravidarum: | Morning Sickness: |
|---|---|---|
| Employment | Often are unable to work for weeks or months and may lose their job or be forced to resign. | May lose up to a month of employment, work part-time and/or use sick time. Job performance may be reduced. |
| Daily Activities | May be unable to perform even simple household chores or care for themselves (shower, drive, etc.) when symptoms are severe. | Can perform most necessary responsibilities at some point during the day or week when symptoms are less intense. |
| Energy Level | Fatigue may be severe for weeks or months. Bed rest is often a necessity. Prolonged fatigue is very common. | Fatigue is mild to moderate and decreases workload. Rest is needed to alleviate symptoms. |
| Relationships & Socialization | Relationships are often greatly strained and may dissolve. Isolation is common and may lead to depression. Abuse and neglect of the mother may occur. | Relationships may be stressed but social functioning is only temporarily reduced. |
| Finances | Financial loss due to medical care, loss of income, and additional paid services (child care) can be devastating. | Financial loss due to medical care, loss of work, and use of sick time is significant, but usually manageable. |
| Stress Level | Psychological stress is typically moderate to severe and often results in anxiety, depression and trauma that may be prolonged. May require treatment. | Psychological stress is mild to moderate and may result in depression during/after pregnancy that may resolve without treatment. |
| Recovery | Postpartum recovery is prolonged, averaging 6 months to 2 years. | Postpartum recovery is typical and usually takes a few months. |
Risks and Outcomes
Most studies examining the risks and outcomes for a pregnant woman with milder nausea and vomiting in pregnancy find no detrimental effects long-term. Those with more severe symptoms that lead to complications, severe weight loss, and/or prolonged nausea and vomiting are at greatest risk of adverse outcomes for both mother and child during pregnancy and in later life. The risk increases if medical intervention is inadequate or delayed.
Treat early and aggressively in mothers with more severe symptoms or with a history of severe symptoms. HG symptoms often worsen with each pregnancy, so use our assessment tools for close monitoring.
Maternal Outcomes
Prolonged HG puts women at greater risk for preterm labor, pre-eclampsia, and long long term complications (often with vague, chronic symptomatology). Acute or chronic complications reported by women to the HER Foundation include gallbladder disease, tempero-mandibular joint disorders, depression, anxiety, difficulty with weight management, diabetes, motion sickness, and dental caries. Some women say they never felt the same as before they were pregnant. Proper intervention in the early stages of HG is essential for maternal health
Fetal Outcomes
According to the medical research, if women fail to gain weight for two consecutive trimesters, it can have detrimental effects on their babies. And women who lose large amounts of weight (>10% of their pre-pregnancy weight) are at greatest risk for maternal and fetal complications, including fetal loss and future neurodevelopmental and behavioral disorders.
Aggressive intervention to control emesis and prevent weight loss is critical.
Psychosocial Impact
Beyond the financial impact, the psychosocial impact is incalculable as many family relationships dissolve and future family plans are limited or pregnancies are terminated. Women often lose their employment because of HG, and women are frequently undertreated and left feeling stigmatized by a disease erroneously presumed to be psychological.
Complications
Although numerous depending on individual biochemistry, severity of symptoms, and medical interventions, many potential complications may result from HG. If care is inadequate, ineffective, or delayed, cases of morning sickness or mild HG may progress to moderate or severe HG. With an aggressive and proactive approach to treatment, many sequelae can be avoided.
Signs of Severe HG
- Debilitating, chronic nausea
- Frequent vomiting of bile or blood
- Chronic ketosis and dehydration
- Muscle weakness and extreme fatigue
- Medication does not stop vomiting/nausea
- Inability to care for self (shower, prepare food)
- Loss of over 5-10% of your pre-pregnancy weight
- Weight loss (or little gain) after the first trimester
- Inability to eat/drink sufficiently by about 14 weeks
Women suffer greatly with HG, and effective intervention early in pregnancy can greatly ease the misery and stress associated with this disease.
Possible Complications
There are many possible complications, however with effective treatment, many can be reduced or avoided.
Causes
There are numerous theories regarding the etiology of hyperemesis gravidarum. Unfortunately, HG is not fully understood and conclusive research on its potential cause is rare. New theories and findings emerge every year, including our collaborative genetics research with UCLA and USC substantiating many cases of HG are caused in part by several genes, and HG is a complex physiological disease likely caused by multiple factors.
Contributing Factors Worsening HG (Hyperemesis Gravidarum)
- Stress/fatigue
- Gastroparesis
- Prenatal vitamins/iron
- Heightened gag reflex
- Excessive salivation
- Helicobacter pylori
- Vestibular sensitivity
- Dysgeusia
- Gall bladder dysfunction
- Dysosmia
- Hormone sensitivity
- Malnutrition
- GERD (Gastroesophageal Reflux Disease)
- Dehydration
Diagnosis
Diagnosis is typically made by measuring weight loss, checking for ketones, quantifying intake and nausea severity, and assessing the overall condition of the mother. However, diagnosis can be confusing for some practitioners if a mother:
- doesn’t produce ketones despite poor intake,
- receives treatment for excessive vomiting such that she does not lose much weight, or
- has severe nausea that makes eating impossible but there is not severe vomiting.
Women in these scenarios likely still have HG, and each woman’s unique symptoms need to be evaluated.
If she meets more than one of the usual criteria (excessive nausea/vomiting, weight loss, dehydration, poor intake, debility) and is having difficulty performing her daily activities, medications and/or other treatments should strongly be considered.
Assessment
Assessing these women can be difficult due to the fluctuations in symptom severity and complexity of their symptoms. Thus, the HER Foundation developed important tools to help you effectively and efficiently evaluate HG patients.
HELP Score
The HER Foundation’s HELP Score is a measurement tool to quantify symptom severity and helps monitor women with more complex symptomatology.
Using patient-friendly language, the HELP Score evaluates the severity of nausea, vomiting and retching, plus five key clinical concerns: hydration, treatment effectiveness and tolerance, psychosocial functioning, oral intake, and overall progress.
Layout allows quick identification of severe symptoms, which will be indicated for answers selected in the far right two columns. Trending the score over time allows more sensitive detection of changes in symptoms.
HG Assessment Packet
The HER Foundation developed a comprehensive assessment packet to promote standardized assessment of HG and improve recognition of comorbidities and developing complications. The Assessment Packet is divided into 3 parts with 1 two-sided page for each section.
- Page 1 is the initial visit assessment and asks questions specific to their previous HG experience and pregnancy history, in addition to child outcomes and postpartum issues. Since symptoms often repeat, this gives you insight into their care requirements.
- The 2nd page is a per visit assessment and allows them to enter their current treatment, intake and symptom details such as date of last bowel movement and appearance of emesis. It includes screening for enteral and parenteral issues, symptoms of other complications associated with HG, and psychosocial difficulties. A question also asks if mothers are considering termination due to HG to alert clinicians to the need for aggressive intervention.
- The 3rd page is a detailed care planning tool for clinicians. It allows them to check off treatments, procedures, labs and educational needs for the patient. Included are many tips and reminders to optimize patient care.
Treatment
Treating HG is very challenging and early intervention usually results in less severe symptoms and better long-term health for both mother and child. Multiple medications are often needed to manage the multitude of symptoms. HG is a multifaceted disease that should be approached with a broad view of possible causes and complications. When treating mothers with HG, preventing and correcting nutritional deficiencies is a high priority to prevent serious complications such as Wernicke’s encephalopathy, and promote a healthy outcome for mother and child.
Nutritional Therapy
Nutrition is one of the most challenging and important issues for women with HG. Pregnant women require a variety of nutrients both for their own healing and for the normal development of their unborn child. The baby's requirements for minerals, vitamins, and other nutrients come first and are taken from the mother's bones, organs, tissues, and other storage areas. This can leave the mother depleted very quickly, which can take months, or even years, to correct.
Therapeutic Abortion
Therapeutic termination is usually avoidable with aggressive treatment of HG. Those who terminate do so most often because of:
Primary Reasons for Termination
- ineffective or inadequate care
- unsympathetic caregivers
- uncontrolled/debilitating HG
- inability to work/care for family
- lost income, job or relationships
- no hope of improving or recovering
The HER Foundation is the leading voice globally offering reserach, support, and treatment resources to reduce the number of women facing this unwanted decision and possible residual trauma.
Early intervention in HG with effective medications can often prevent the need for abortion. Unfortunately, the medications most effective have the least amount of research and a short history of use in pregnancy. Many practitioners are hesitant to use them. Further, confusing and somewhat misleading studies create concern over risks.
Risks of Therapeutic Termination
Women left untreated sometimes become so metabolically imbalanced, termination is chosen to save the life of the mother who is facing organ failure. In other cases, the mother and child are put at high risk for serious and potentially life-long complications. Therapeutic abortion should be considered only as a last resort.
The numerous potential adverse effects of abortion cannot be overlooked or underestimated. It is well-known that there are physiological and psychological repercussions for abortions, and these increase in women with repeat abortions. Aborting a wanted child can create debilitating, long-term psychological impact.
Support After Loss
Read stories of women who terminated due to HG on the Shadowlands forum, and view HER Loss Support Group and volunteers who have experienced loss to offer emotional support. When requesting to join the HER Loss Support group, please answer the questions.
Elective pregnancy termination in a large cohort of women with hyperemesis gravidarum.
Results: Of 808 women who completed the survey, 123 (15.2%) had at least one termination due to HG, and 49 (6.1%) had multiple terminations. Prominent reasons given for the terminations were inability to care for the family and self (66.7%), fear that they or their baby could die (51.2%), or that the baby would be abnormal (22.0%). These same women were three times as likely to state that their health care providers were uncaring or did not understand how sick they were [64/123 (52.0%) vs. 168/685 (24.5%), odds ratio 3.34 (95% CI 2.21–5.05), pb.001].
Conclusion: These data suggest that the physical and psychological burden of HG has been underestimated, and that further education within the medical community may be warranted.
Source: Contraception 76 (2007) 451–455
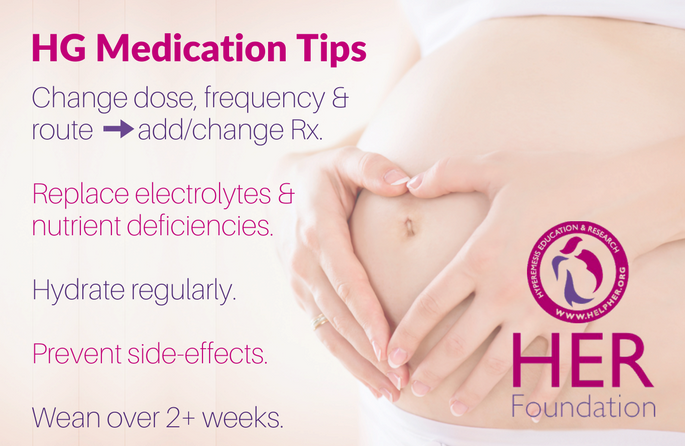
Medications & Tools
Numerous medications are available to target various comorbid symptoms such as reflux, gastroparesis and vomiting. Mothers often need multiple medications to target these symptoms for adequate relief. Research has found better outcomes in those receiving medications and nutritional intervention than in those who try to avoid medications. Our Medication Strategies brochure provides expert insight into managing medications.
Safety
Taking medications during pregnancy can be very upsetting for women as the general belief is that they will hurt their baby(ies). However, the stress and risks of chronic dehydration, malnutrition, metabolic and emotional stress, as well as reduced mobility will generally develop. These have been demonstrated to increase the risk of complications in mothers and possibly even in their child(ren). Conversely, most studies of medications commonly used for HG have not been found to significantly increase the risk of malformations in the baby.
Non-oral Medications
It is important to not only decide on the correct medication, or combination as is most common, but also to make sure a medication is being tolerated and taken correctly for optimal effectiveness. If a mother cannot swallow a pill or vomits it back up before it dissolves, then oral medications need to be replaced with medications that can be given a different route until a mother is more stable. Some medications can be made into a different form, such as a cream or suppository, by a compounding pharmacy. Others are available as oral dissolvable tablets/films, patches, or suppositories.
Trying the most effective medications in different forms is important before trying different medications, or deciding medications do not work.
"Keep in mind, the primary goal of treatment is to reduce nausea and vomiting, so the mother can increase her intake and stay as mobile as possible. Risks and benefits must be considered in every case as each pregnancy is unique."
- Kimber MacGibbon, RN -
HG Protocol & Algorithm
Over the last 20 years of research and patient advocacy, the HER Foundation has developed insight into the practical management of HG to optimize patient response and outcomes. Using this knowledge, we have developed an HG Treatment Protocol and Algorithm to guide you in managing HG. While we advocate for proactive care and earlier transition to non-oral medication administration, our treatment recommendations are compatible with those of the American College of Obstetricians and Gynecologists.
Source
- Ondansetron in Pregnancy and Risk of Adverse Fetal Outcomes. N Engl J Med 2013; 368:814-823.
- Risk factors, treatments, and outcomes associated with prolonged hyperemesis gravidarum. J Matern Fetal Neo Med. 2012 Jun;25(6):632-6.
- Posttraumatic stress symptoms following pregnancy complicated by hyperemesis gravidarum. J Matern Fetal Neo Med. 2011 Nov;24(11):1307-11.
- Symptoms and pregnancy outcomes associated with extreme weight loss among women with HG. J Women’s Health. 2009 Dec;18(12):1981-7.
For more information: www.hyperemesis.org/hyperemesis-research/
Postpartum Recovery
Recovering from hyperemesis gravidarum (HG) takes an average of 4-6 months, but may take a few years if her illness was severe or prolonged. Some women will have residual issues long-term, sometimes with vague or atypical immune or gastrointestinal symptoms that are difficult to resolve.
Recovery Time
Women who have nausea/vomiting into late pregnancy usually find it takes months to regain their energy and restore their nutritional reserves. Food aversions may persist and take months or even years to overcome. It will often take 1-2 months of recovery for every month she was malnourished or debilitated by HG. Any additional complications during pregnancy should be re-evaluated postpartum by a primary care doctor to ensure complete recovery.
Mental Health
Women diagnosed with HG have an increased risk of Perinatal Mood and Anxiety Disorders (PMADs) and Post Traumatic Stress Disorder (PTSD). Families need to be aware of common postpartum issues and their symptoms to ensure women get the care they need. A mother’s health greatly impacts the development of her child(ren).
Impact on Society
Hyperemesis Gravidarum is more than a pregnancy illness that impacts patients and their families. HG impacts society. Conservative estimations suggest HG costs nearly $500 million annually just for inpatient hospitalization. There are also over 375,000 outpatient visits to emergency rooms for treatment of HG at an estimated cost of $2.5 billion, plus home health care, pharmaceuticals, outpatient infusion care, diagnostics, and frequent obstetrical visits. Considering so many HG patients are treated outside the hospital to save costs, the actual cost is many times greater. The costs for HG treatment exceed $3 billion for HG each year in the US, and many get inadequate care. The long-term effects of HG and its complications add many $1000's in costs over time.

